Coombs test is also known as antiglobulin test. The Coombs test tests for antibodies that may stick to the red blood cells and cause red blood cells to die too early. It was discovered by Coombs, Mourant and Race in 1945. Coombs reagent is antihuman globulin. It is made by injecting human globulin into animals, which produce polyclonal antibodies specific for human immunoglobulins and human complement system factors.
Principle of Coombs test
Red cells coated with complement or IgG antibodies do not agglutinate directly when centrifuged. These cells are said to be sensitized with IgG or complement. In order for agglutination to occur an additional antibody, which reacts with the Fc portion of the IgG antibody, or with the C3b or C3d component of complement, must be added to the system. This will form a “bridge” between the antibodies or complement coating the red cells, causing agglutination.
Types of Coombs test
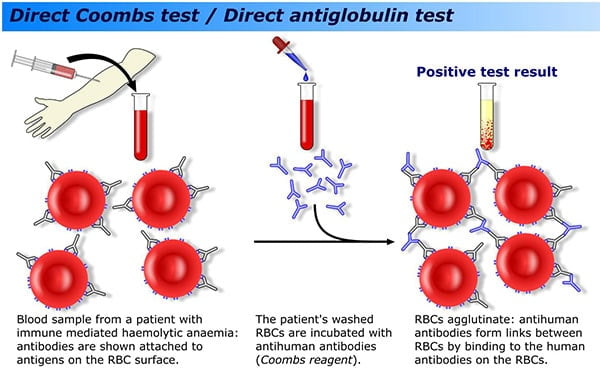
Direct Coombs Test (Direct Antiglobulin Test- DAT)
The direct Coombs test is used to detect antibodies (IgG or C3) that are stuck to the surface of red blood cells. Many diseases and drugs can cause this. These antibodies sometimes destroy red blood cells and cause anemia.
This is the test that is done on the newborn’s blood sample, usually in the setting of a newborn with jaundice. The two most commonly recognized forms of antibody-mediated hemolysis in newborns are Rh incompatibility and ABO incompatibility.
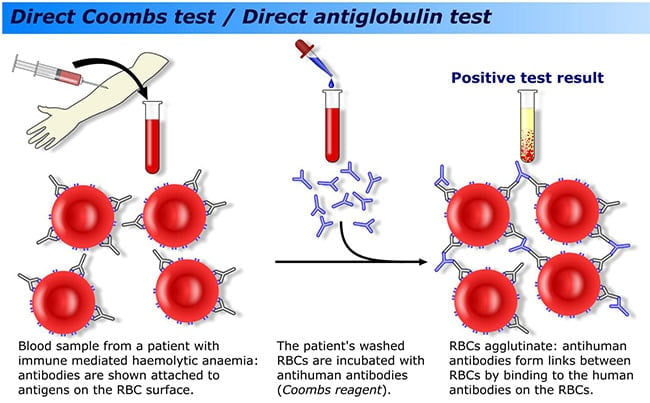
Procedure of Direct Coombs Test
- Prepare a 5 % suspension in isotonic saline of the red blood cells to be tested.
- With clean pipette add one drop of the prepared cell suspension to a small tube.
- Wash three times with normal saline to remove all the traces of serum.
- Decant completely after the last washing.
- Add two drops of Anti-human serum.
- Mix well and centrifuge for one minute at 1500 RPM.
- Resuspend the cells by gentle agitation and examine macroscopically and microscopically for agglutination.
Indirect Coombs Test (Indirect Antiglobulin Test- IAT)
The indirect Coombs test looks for free-flowing antibodies against certain red blood cells. It is most often done to determine if you may have a reaction to a blood transfusion.
This is the test that is done on the mother’s blood sample as part of her prenatal labs. Frequently referred to as the “antibody screen”, this test identifies a long list of minor antigens that could either cause problems in the newborns or cause problems in the mother if transfusion is necessary.
Approximately 5% of patients have a positive IAT due to IgG antibodies, IgM antibodies, or both.
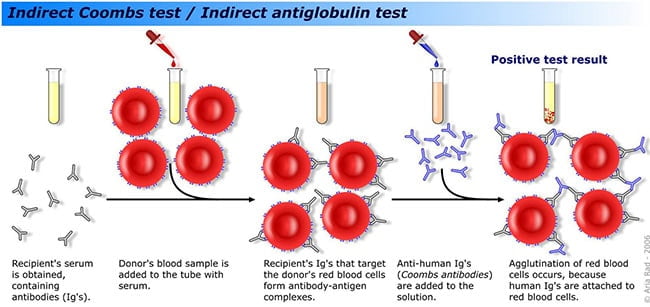
Procedure of Indirect Coombs Test
- Label three test tubes as T (test serum) PC (Positive control) and NC (negative control).
- In the tube labeled as T (Test), take 2 drops of test serum.
- In the test tube labeled as PC (Positive control), take 1 drop of anti D serum.
- In the test tube labeled as NC (Negative control), take 1 drop of normal saline.
- Add one drop of 5 % saline suspension of the pooled ‘O’ Rho (D) positive cells in each tube.
- Incubate all the three tubes for one hour at 37°C.
- Wash the cells three times in normal saline to remove excess serum with no free antibodies, (in the case of inadequate washings of the red cells, negative results may be obtained).
- Add two drops of Coombs serum (anti human serum) to each tube.
- Keep for 5 minutes and then centrifuge at 1,500 RPM for one minute.
- Resuspend the cells and examine macroscopically as well as microscopically.
Result Interpretation of Coombs Test
Negative Result:
No clumping of cells (no agglutination). This means you have no antibodies to red blood cells.
Positive Result:
Clumping (agglutination) of the blood cells during a direct Coombs test means that you have antibodies on the red blood cells and that you may have a condition that causes the destruction of red blood cells by your immune system (hemolysis). This may be due to
- Hemolytic anemia,
- Chronic lymphocytic leukemia or similar disorder,
- Erythroblastosis fetalis (hemolytic disease of the newborn),
- Infectious mononucleosis,
- Mycoplasmal infection,
- Syphilis,
- Systemic lupus erythematosus and
- Transfusion reaction, such as one due to improperly matched units of blood.
References:
- Stanford School of Medicine
- Institute For Transfusion Medicine
- Johns Hopkins Lupus Center
- University of Alberta
- Madison College
- Healthline
- Medline Plus
- Web MD
- Lab Test Online
- Patient
- Cigna
- Medscape
- Healthlink BC
- Laboratory Info
- Wikipedia
My indirect coomb test came out positive and am 20 weeks pregnant, my Doctor said not to worry but I’m still concerned. What else can I do?
What does weak positive IDAT Test result means?
I did direct and indirect coombs test today and it all came out negative. Please do I still have to go for Rhogam injection because I still want to have a baby.
please mention blood group of mother and baby ; is this your first or second pregancy;whether you had any previous history of rhogum injection
Are you Rhesus D negative? If yes, with the results you got, it means that you are not yet sensitized to produce anti-D. Therefore, if carry a Rhesus D positive pregnancy in the first instance, that foetus will be free from Haemolytic Disease of the Foetus and the Newborn
However, your Obstetrician may give you Rhogham post delivery to prevent you from being sensitized
I hope this helps
Can You Please explain the quantities in micron? is one drop equals 50 micron?
and please explain how you resuspend in step 10?
why it is a need to incubate sample in doing the Indirect Coomb’s Test?
Nice explanation.But I have a doubt that why we r adding O pooled cells only ,we can use A or B also no ?
No we can’t since these A or B cells have antigens coated on their RBC surface hence may interfere the results but for O positive cells , they don’t have any antigen except the Rh antigens which is important in the testing
O cells lack the A and B antigens and will therefore not cause any discrepancy with the naturally occurring antibodies A an B
My indirect coombis test result are positive (grade 4+). Please help me.
Hallo Payal, since your indirect coomb’s test is positive, you need to find out what is reponsible as there are a long list of antibodies – Anti D, C, E, Lewis, Duffy, etc – that could cause that. That helps you to prevent transfusion problem, whenever you might need blood. And if you are still able to bear children, knowing the cause of your positive IAT will prevent the chances of having miscarriage or any post-natal complications, because of medical intervention you would receive. hope that helps.
POSITIVE CONTROL- use antibody-coated cells, which are commercially available or maybe prepared in the laboratory
NEGATIVE CONTROL – known non-sensitized cells serve as negative control
RMT from PH
Great presentation. I used to work in the blood bank as a medical technologist performing DAT and IDAT testing. This presentation is simple and to the point. This was a good review for me.
I have a doubt, “how can antibodies bind to cell O if has no antigens”. Since we know the antibodies bind to antigen to recognize as a foregin particle.
sir, actually in coombs test there is a negative result means? pls clear my doubt.
@Sandy. A negative result means that the complement was not fixed to prevent agglutination.
It equally implies that the antibodies (Ab) were not sensitized.
provided the test was done acccurately, negative result simply means you do not have any foreign immune antibody on your cells, that could cause immune reaction (agglutination reaction). It could also be that the titre value of the antibody is too low to be detected. This is usually the case with people who had received anti-D prophylaxis in the past.
ICT:Three tubes T,NC,PC In tube T:pt serum+O pooled cells. Tube NC:O Dneg cells+ anti D antisera 1/5 diluted. Tube PC:O Dpos cells+ anti D antisera 1/5 diluted.
in ict there was error in procedure.no human serum was used.so which blood do we use to test for cell sensitization in vitro.but good notes in DCT.
Can u tell me that whether this test is altered by steroid therapy
as far as i could remember, there has been no study to establish this. but since steroid therapy relates to immune system, one can not completely rule out the effect on the ICT especially.
There is not clearly verify that how to make negative and positive controls
Bt there is no clearly verify of negative control
i didn’t recognise the third tube.
Very fantastic descriptions of reaction bt error in ICT procedure step 2&3 instead
1 Test tube label T serum
2 Test tube label PC Anti D
3Test tube label NC saline
to save yourself this hurdle, just buy a commercially prepared ICT test kits.
We have developed a new Superagglutination test for serodiagnosis of infectious diseases. It differs from conventional plate/slide agglutination tests (PAT/SAT) by three additional steps: prior staining of serum antibody by adding a dye and addition of diluted biotinylated antiglobulin and avidin in sequence after mixing the antigen with the test serum. The new steps circumvent the problems of false positive and false negative results of PAT/SAT. In serodiagnosis of brucellosis, Superagglutination test had higher positive predictive value and specificity than Rose Bengal Plate Test (RBPT) and Standard Tube Agglutination Test (STAT) and higher negative predictive value and sensitivity than RBPT, STAT, ELISA and Complement Fixation Test (CFT).
Read the full paper at:
http://www.sciencedirect.com/science/article/pii/S2215016115000424
doi:10.1016/j.mex.2015.08.001
is there a kit for super agglutination test
It has been several years since I have worked in BB is there now a completely automated way to do a Coombs test? A more general question can a cross match NOW be done by machine….or is it still the familiar labor intensive procedure I am familiar with?
With Respect
Seth Malovany MT AMT