- Different bacteria produce an important class of enzymes called beta-lactamases, which may be mediated by genes on plasmids or chromosomes.
- These enzymes confer resistance to a number of penicillin antibiotics by cleaving the beta-lactam ring of penicillins and cephalosporin antibiotics, resulting in inactivation of these drugs.
- They are capable of inactivating “penicillinase-labile-penicillins”, such as amoxicillin, ampicillin, penicillin, carbenicillin, mezlocillin, and piperacillin.
- β-lactamases thus play a key role in bacterial resistance to beta-lactam agents, and detection of their presence can provide useful information.
- Various assays are available to detect β-lactamases, such as the iodometric method, the acidometric method, and by the use of chromogenic substrates.
Objective
To detect the enzyme beta-lactamase, which confers penicillin resistance to various bacterial organisms.
Principle
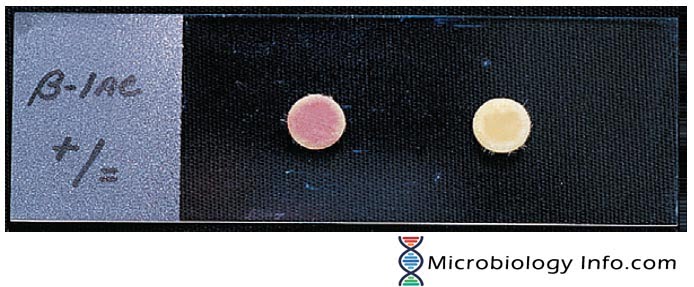
One of the most useful tests in clinical laboratories for β- lactamase detection is the chromogenic cephalosporinase test. The test disk employed consists of a chromogenic cephalosporin which is used as the substrate. Organisms possessing β-lactamases when applied to the disk, exert their effect by opening the β-lactam ring of the substrate. This process results in a colored product which is conspicuous and hence allows detection. On hydrolysis by the bacterial inoculum, a deep pink color is produced. Lack of color production indicates the absence of β-lactamase.
Test Disk
- The Cefinase disk is an example of a commercially available chromogenic test (BD Microbiology Systems, Cockeysville, Maryland).
- The disk incorporates nitrocefin as the substrate.
- It exhibits a very rapid color change from yellow to red as the amide bond in the beta lactam ring is hydrolyzed by a beta-lactamase.
- When a bacterium produces this enzyme in significant quantities, the yellow-colored disc turns red in the area where the isolate is smeared.
Method
- Using a single disk dispenser, dispense the disk from the cartridge into an empty petri dish or onto a microscope slide.
- Moisten disc with 1 drop of sterile distilled water.
- With a sterilized loop or applicator stick remove several well-isolated similar colonies and smear onto a disk surface.
- Observe disk for color change.
Expected Results
- Positive: Yellow to pink-red color change on the area where the culture is applied.
- Negative: No color change.
Uses
Useful applications include detection of:
- N. gonorrhoeae resistance to penicillin
- H. influenzae resistance to ampicillin
- Staphylococcal resistance to penicillin
Limitations
- Application of tests to directly detect β-lactamase production is limited to organisms producing enzymes whose spectrum of activity is known. This also must include the β-lactams commonly considered for therapeutic eradication of the organism.
- It is not supposed to entirely replace conventional susceptibility test methods, as other factors also influence the results of such tests.
- Detection of beta-lactamase activity in staphylococci may take up to one hour.
- Each disc is used to test one bacterial strain for the presence of beta-lactamase.
References
- Tille, P. M., & Forbes, B. A. (2014). Bailey & Scott’s diagnostic microbiology (Thirteenth edition.). St. Louis, Missouri: Elsevier.
- Murray P.A., et al. Manual of Clinical Microbiology, 7th ed. 1999.
- www.asmscience.org/content/book/10.1128/9781555817435.chap5.3
- https://eportal.mountsinai.ca/Microbiology/manual/tech/tech06.pdf
My sinus culture indicates H. Influenza beta lactamase negative. I have tried several anti-biotic therapies. Including Ceftazidme nasal irrigation, Cefuroxime axetil orally with no results . Can some one please advise or suggest a better approach for treatment? Would an injection be more effective. This is mostly a sinus and throat centered infection. Any input would be helpful. I had sinus culture done by the ent that indicated H . Influenza . I had the PCR test but without susceptibility test. Should I get a Next Generation Sequence done to further identify the organism?