The eventual death toll from the massive earthquake that struck Nepal on April 25 will be unbearable. The death toll from Saturday’s deadly 7.9 magnitude quake and a series of aftershocks that struck various parts of Nepal has reached 4347 leaving 8154 injured as of Tuesday morning.
The overwhelming majority of deaths immediately after a natural disaster are directly associated with blunt trauma, crush-related injuries and burn injuries. The risk of infectious disease outbreaks in the aftermath of natural disasters has usually been overemphasized by health officials and the media, leading to panic, confusion and sometimes to unnecessary public health activities.
The risk factors for increased infectious diseases transmission and outbreaks are mainly associated with the after-effects of the disasters rather than to the primary disaster itself or to the corpses of those killed. These after-effects include displacement of populations (internally displaced persons and refugees), environmental changes and increased vector breeding sites. Unplanned and overcrowded shelters, poor water and sanitation conditions, poor nutritional status or insufficient personal hygiene are often the case. Consequently, there are low levels of immunity to vaccine-preventable diseases, or insufficient vaccination coverage and limited access to health care services.
With the lack of safe drinking water and sanitation after the April 25 earthquake, people in Khokana village, the southern outskirt of the Kathmandu Valley, has begun suffering from diarrhoea. Outbreaks have also been related to shared water containers and cooking pots, scarcity of soap and contaminated food, as well as pre-existing poor sanitary infrastructures, water supply and sewerage systems.
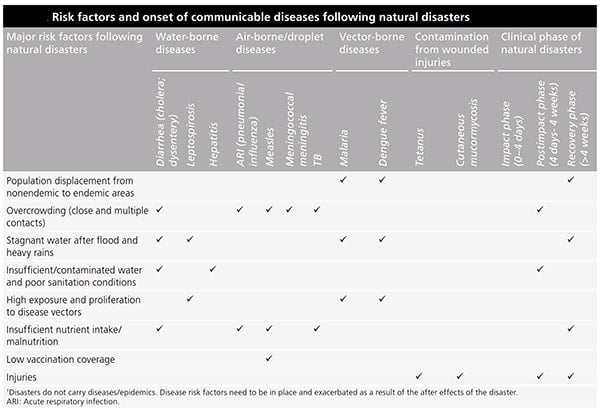
The most common causes of morbidity and mortality in this situation are diarrheal disease and acute respiratory infections.
Waterborne diseases:
Diarrheal disease: Diarrheal disease outbreaks can arise subsequent to drinking-water contamination, and have been reported after flooding and related movement. Vibrio cholera (O1 Ogawa and O1 Inaba) and enterotoxigenic Escherichia coli are the major causes of this type.
Hepatitis A and E: Hepatitis A and E have also fecal-oral transmission, especially in poor water sanitation.
Leptospirosis: Leptospirosis is a bacterial zoonosis transmitted through contact of mucous membranes and skin with water, moist vegetation, or dirt contaminated with rodent urine.
Diseases associated with crowding:
Acute respiratory infections (ARI) as the main cause of morbidity and mortality among unsettled people are seen predominantly in children less than 5 years old. Furthermore, meningitis and measles are transmitted from person to person, especially in crowded circumstances.
Vector-borne diseases:
Malaria, cutaneous leishmaniasis and rabies are transmitted by vectors.
Infections due to wounds and injuries:
The potentially significant threats to persons suffering a wound are tetanus, staphylococci and streptococci.
Prevention and control measures
- Hand-washing with soap after handling bodies and before eating, use and correct disposal of gloves and use of body bags if available.
- Always use a face mask. Cover your mouth and nose with a tissue when coughing or sneezing.
- Always drink a boiled and filter water.
- Shelters should have sufficient space according to the needs of victims. Furthermore, access to the water, fuel, and transport, solid waste management, and safety of food stores are essential.
- According to WHO guidelines, Chlorine is broadly obtainable, low-cost, easily used and effective against almost all waterborne pathogens. People should have sufficient facilities and provisions to collect, save and use adequate quantities of water for drinking, cooking and personal hygiene, and to certify that drinking water remains safe until consumption.
- Ensure food is stored, cooked, prepared and served in a hygienic manner.
- The importance of soap and hand washing as a protection against fecal-oral disease should be emphasized in educational programs. Soap and water should be provided to all disaster victims and rescue personnel.
- Vector control interventions based on the local context and epidemiology of diseases are essential. Examples of some useful interventions are indoor residual spraying for malaria, insecticide-treated nets, and traps for tsetse flies as the vectors of trypanosomiasis.
- Awareness of the emergence of water and food born disease is of importance to the health of the victims.
- More attention should be paid to early diagnosis and treatment of multiple infections and special infections in survivors of natural disasters. One such infection, gas gangrene, is an acute, severe, life-threatening disease for which early diagnosis is critical.
- Waste disposal should comply with local requirements including disposal of regulated medical waste such as syringes and needles.
- We recommend re-establishing and improving the delivery of primary health care.
- Medical supply should be provided, and training of healthcare workers and medical personnel on appropriate case management should be conducted.
- Education on hygiene and hand washing, and provision of an adequate quantity of safe water, sanitation facilities and appropriate shelter are very important for prevention of infectious diseases.
Similar Posts:
- Cryptococcus Neoformans – Habitat, Morphology, Epidemiology, Virulence Factors, Treatment + More
- Hepatitis B Virus- Structure, Epidemiology, Symptoms, Pathogenesis, Diagnosis, Treatment and Vaccines
- Scrub Typhus- Etiology, Epidemiology, Symptoms, Pathogenesis, Diagnosis and Treatment
- Alternaria Alternata – Habitat, Morphology, Epidemiology, Pathogenesis, Laboratory Diagnosis + more