Habitat
Alternaria alternata is mainly an outdoor fungus
- Alternaria alternata is mainly an outdoor fungus whose spores disseminates in warm, dry air, so in temperate climates and found at higher concentration in dry windy conditions.
- It may also be found in damp, insufficiently ventilated houses.
- Its exposure is often assessed by outdoor spore counts, because most intense exposure is likely to occur in an outdoor environment.
Alternaria, is a fungus whose spores occur worldwide in
- The spores can be found in the organic constituents of soil throughout the year and in organic materials in damp situations including textiles, stored food, canvas, cardboard and paper, electric cables, polyurethane, jet fuel, sewage and effluents.
- In seasons from spring to autumn, they become airborne and are therefore even more ubiquitous.
- It is also commonly isolated from plants and food.
Morphology
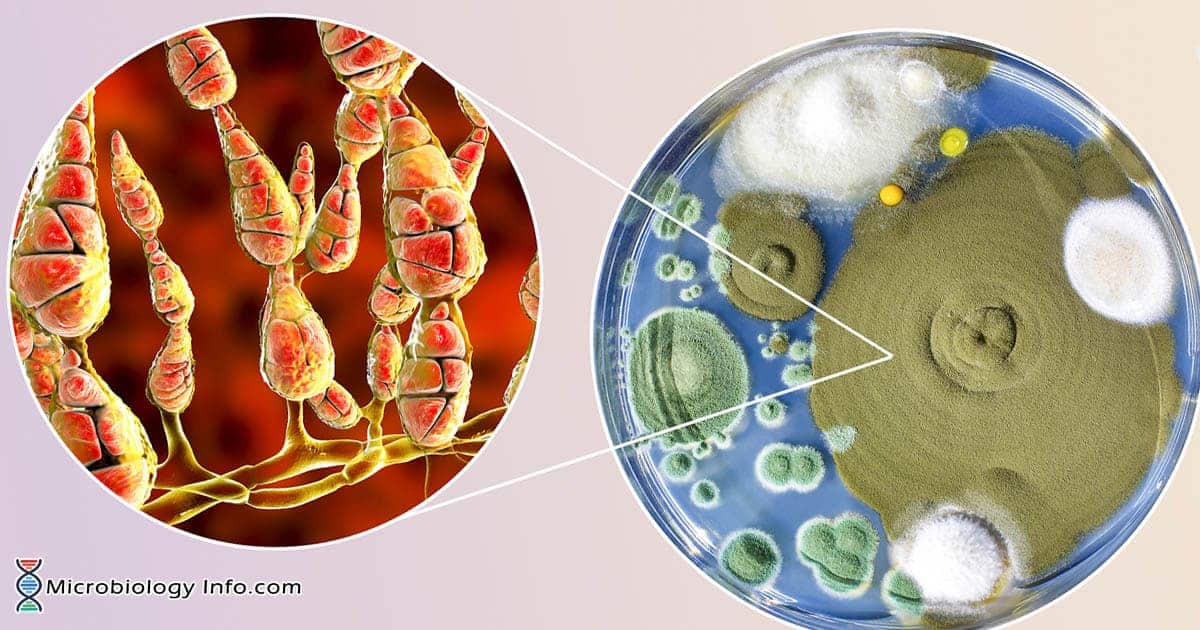
- Alternata forms fast-growing colonies in dark colors ranging from gray to olive or olive brown.
- The surfaces of mature colonies appear “fuzzy,” “downy to wooly,” or “suede like” due to the presence of numerous hyphae.
- Microscopic observation shows the brown septate hyphae form conidiophores, which are also septate.
- Conidia found are either single or forming chains, are simple and large, with the size 45–50×36 μm.
- While in natural habitats, the conidia are larger, more uniform, and have elongated tips in comparison to those grown on agar media.
- The cells are surrounded by cell walls consisting of chitin and β-1,3-glucans.
- The fungus produces dry, relatively large spores measuring 25–56×8–17 μm which are “beak like,” elongated, and transversially septated.
- The spores separate from the conidiophore in dry air both passively and under the influence of strong gusts of wind.
- Humid conditions of 84–89 and 97 % facilitates both growth of fungi and production of mycotoxins.
Epidemiology
- Alternaria alternata are classified and termed as “outdoor” molds which occur cosmopolitically in various environments and worldwide in distribution.
- Its spores are common aeroallergens in many regions of the world, especially in warm inland climates, but also in arid regions.
- It occurs more often in warm climates such as in the Mediterranean.
- In the subtropic and tropic zonal areas, spore counts remain significantly high throughout the year.
- In temperate climates, the spores mainly occur from May to November and the spore counts peak in late summer and autumn.
Pathogenesis
- The portal of the entry is inhalation of the spores circulating in the environment.
- In hypersensitive patients, allergens are responsible for causing a particular allergic reaction.
- The enzyme proteases released from alternata induce the activation and degranulation of human eosinophils which is one of the immune system components responsible for controlling mechanisms associated with the development of allergy and asthma.
- Additionally, eosinophil granulocytes are activated through the protease-activated receptor 2 (PAR-2) which is involved in the recognition of the antigens.
- This further leads to the phenomenon of opening of the tight junctions in the epithelium.
- Subsequently, human epithelial cells as a response to stimulation produce biologically important cytokines and growth factors, including IL-6, IL-8, and also GM-CSF which are released during allergic reactions and play a significant proinflammatory role.
- The allergen also enhances lung eosinophilia, peribronchial infiltration, and epithelial mucus production, which may lead to the development of severe asthma.
Clinical Manifestations
- Alternata is responsible for the allergic symptoms in individuals with rhinitis or bronchial asthma.
- Alternaria sensitivity can further lead to severe and potentially fatal asthma in some individuals.
- The threshold concentration of fungal spores for allergic reactions to occur is 80 spores/m3 of air with the clinical symptoms occurring in the first sensitized patients.
- At 100 spores/m3, all the sensitized patients develop symptoms, while at 150 spores/m3 , the symptoms exacerbate and 300 spores/m3 dyspnea appears.
- It is also found as an opportunistic pathogen causing skin diseases particularly in immunocompromised patients such as the bone marrow transplant patients.
- The fungal spores and/or mycelial cells cause type I allergy which is the most prevalent disease.
- In addition, it also causes a large number of other illnesses, including allergic bronchopulmonary mycoses, allergic sinusitis, hypersensitivity pneumonitis, and atopic dermatitis and fungal allergies are frequently linked with allergic asthma.
- Alternaria alternata is one of the rarest fungi associated with paranasal osteomyelitis.
- Most infections in humans occur in immunologic impairment patients and far less often in healthy individuals.
- The clinical spectrum of the disease includes the following: Hypersensitivity pneumonitis, granulomatous lung disease, bronchial asthma, paranasal sinusitis with and without osteomyelitis, allergic sinusitis and rhinitis, keratitis, peritonitis and cutaneous and subcutaneous deep-tissue infection.
- Avery rare case of visceral Phaeohyphomycosis caused by the opportunistic fungus Alternaria alternata involving the left kidney of the patient is also found.
Laboratory diagnosis
Specimens: sputum, pus, skin scrappings, tissue
Microscopy
- Microscopic examination of stained clinical specimens shows characteristics of alternate; conidiophores arise from septate hyphae, the conidia are obclavate, pyriform to ovoid or ellipsoidal up to 50 mm long and 3-12 mm wide, medium-brown with a short, cylindrical beak, and form long and profusely branched chains (ten or more conidia).
- Upon histological examination, Alternaria shows more or less irregular melanized hyphae.
Culture
- Clinical material should be inoculated on Sabouraud glucose agar or Sabouraud dextrose agar and incubated at 25-30°C.
- The dark brown or olivaceous to black mould colonies are formed within 1-2 weeks, but cultures should be retained for at least 4 weeks before being discarded.
Molecular detection
- The use of molecular techniques facilitates the identification of Alternaria using the Basic Local Alignment Search Tool (BLAST) which allows comparing sequences of a given unidentified fungus with those deposited previously in GenBank in order to find regions of similarity among sequences.
- PCR based method using general primers can also be used.
Treatment
- The cases of disease caused by Alternaria alternata is treated with the older antifungal drugs, e.g. amphotericin B, flucytosine, fluconazole, miconazole and nystatin.
- Itraconazole has been used most frequently in cases of onychomycosis and cutaneous and subcutaneous infections. However, voriconazole could be a good alternative.
Prevention
- Fumigation could reduce the circulation of the fungal spores in the hospital environment.
- Contact with soil or trauma of the nails are the most frequent predisposing factors for onychomycosis caused by Alternaria, hence walking barefoot on the farming area should be avoided.
- Postharvest control of alternata diseases in fruits and vegetables by using conventional methods as well as a number of novel strategies including biological control, heat treatment, natural compounds (chitosan, isothiocyanates, essential oils, elicitors of natural defense mechanism) can be done.
References
- Richardson M.D and Warnock D.W. (2003). Fungal Infection- Diagnosis and Management. Third edition. Blackwell Publishing Ltd. Page 336-344.
- Salo, P. M., Yin, M., Arbes, S. J., Cohn, R. D., Sever, M., Muilenberg, M., Burge, H. A., London, S. J., Zeldin, D. C. 2005. Dustborne Alternaria alternata antigens in US homes: results from the National Survey of Lead and Allergens in Housing. The Journal of allergy and clinical immunology, 116(3), 623-9.
- Salo, P. M., Arbes, S. J., Sever, M., Jaramillo, R., Cohn, R. D., London, S. J., & Zeldin, D. C. 2006. Exposure to Alternaria alternata in US homes is associated with asthma symptoms. The Journal of allergy and clinical immunology, 118(4), 892-8.
- Kustrzeba-Wójcicka I, Siwak E, Terlecki G, Wolańczyk-Mędrala A and Mędrala W. 2014. Alternaria alternata and Its Allergens: a Comprehensive Review. Clinic Rev Allerg Immunol. DOI: 10.1007/s12016-014-8447-6.
- Pastor J and Guarro J. 2008. Alternariainfections: laboratory diagnosis and relevant clinical features.
- Chhabra V, Rastogi S, Barua M, Kumar S. 2013, Alternaria alternata infection associated osteomyelitis of maxilla: A rare disease entity. India J Dent Res; 24:639-41.